by: Josh O’Dell/Geomagic Solutions
Twenty-seven years ago doctors suggested that Barry Fell have a knee replacement to fix his worn out knee. However, “I didn’t like it,” he said. “The high success rate with stock implants has to do with alleviating pain. But with a manmade replica of a knee, in terms of structure, ligaments, and so on, it’s not even close to what you’re giving up. You can’t do what you did before. And once you get the implant, there’s no going back.” He decided to wait until there was better technology for his knee. And in fact, decided that he should be the one to create it. So with his graduate degree in chemistry and years of experience in the textile and aerospace industries, he jumped into orthopedics.

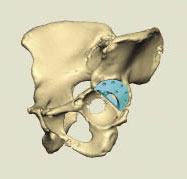
Displaced cage hip dislocation visualized in Geomagic Freeform direct from CT scan data.
Most surgeons were comfortable with stock, one-size-fits-all implants. “But,” Fell said, “custom is better.” His small mission has morphed into a full-fledged business. And the industry has started to come around, largely due to the successful outcomes produced by his company, Thermoplastic Products Corporation (TPC) of Hummelstown, Pa.
Fell uses a combination of Geomagic Freeform 3D modeling software, CAD, and rapid prototyping/additive manufacturing techniques on some of the most challenging implant cases. He relies heavily on Geomagic Freeform because it gives him the ability to sculpt 3D clay models using a touch-enabled interface and to construct them quickly. As they are essentially extensions of the human body, organic components in and of themselves, implants and surgical guides require a high degree of design freedom. They require the ability to shape natural, curved solids, which Freeform delivers.
“Freeform manipulates .stl’s like nothing else can,” said Fell. “There’s not another good way that we’ve found in terms of speed and efficiency.”

Creating the cup design to safely house the hip joint.
A previously active 60-year-old, only four months removed from her second hip implant, was admitted to the hospital in extreme pain. Osteoporosis and bone erosion had caused the implant cup to dislodge and collapse into her pelvis, resulting in a severely dislocated hip and allowing the implant cup to tread dangerously close to vital organs.
Doctors at the Orthopedic Institute of Pennsylvania determined that a third implant in her continually eroding, delicate pelvic bone would be most successful if they used a then-new trabecular metal material. Trabecular metal encourages new bone cells to grow into the implant itself rather than relying on screws and the usually heavy volume of cement to keep the cup in place.
However, at the time, custom trabecular metal implants had a 24-week development window, due largely to the effort required to create the material itself. In that amount of time, however, her anatomy would change and the custom implant wouldn’t fit. A 24-week wait was too long.
Placement of the designed augment in the hip.
TPC cut it to two days. Using Geomagic Freeform, they altered an off-the-shelf trabecular implant cup prior to surgery and provided pre-surgical visualization. The result: Surgeons didn’t have to alter it in the operating room, and the patient wasn’t exposed to infection and anesthesia for long periods of time.
After converting the patient’s CT scan into an .stl file, TPC engineers used Freeform to make a mirror image of her healthy right hip to use as an overlay for the damaged left. Able to see where her pelvic bone and femur naturally aligned, engineers designed, sourced, and provided the required cup implant and augments for surgery in two days. The design took less than an hour. Because Freeform includes four different modeling representations – voxels, NURBS, polygons, and SubD – TPC engineers were able to work in the right mode for a given task while altering and reshaping components for fit.
To verify accuracy, the engineers used Freeform to fit the cup within the patient’s virtual 3D pelvic structure. Once
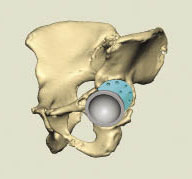
Placement of the cup and augment to fully protect the hip.
the design was complete, Freeform’s measurement functions allowed the engineers to verify that an off-the-shelf acetabular cup and set of augments would be suitable in creating the final implant.
Freeform and its realistic touch-based interface allowed surgeons to review and practice the surgery on an exact virtual model of the patient’s anatomy. This preparation was vital considering that the patient’s flimsy existing pelvic bone measured anywhere from 20 mm in spots to a mere 1 mm in others. The surgeons used Freeform and haptic devices with force feedback to physically feel the simulations they were performing on screen. They were able to detect points of resistance as they placed long rods through the proposed screw holes and verify that the hardware would retain the new cup in her dangerously thin pelvic structure.
Once the design was complete, TPC engineers provided measurements and made a 3D-printed study model for the surgeon’s final approval. This model was also useful, as it functioned as a reference during the surgery.
Geomagic, 3D Systems
www.geomagic.com/en/
Filed Under: Medical-device manufacture



Tell Us What You Think!